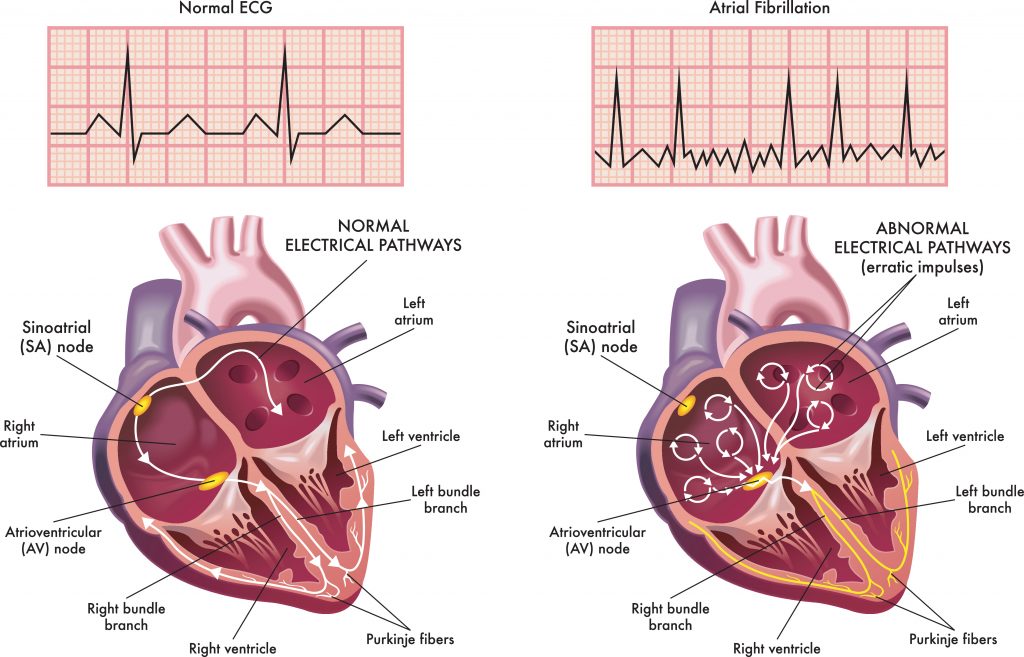
What Is Atrial Fibrillation?
Atrial fibrillation is a common heart rhythm disorder caused by irregular electrical signals in the upper chambers of the heart. It affects millions of Americans and increases the risk of stroke, heart failure, and other complications. Managing AFib often means a combination of lifestyle adjustments and ongoing medication, so understanding drug interactions is essential for heart health[1].
Why Medication Choices Matter
With new medications and remedies available every year, paying attention to medication safety is critical for those with AFib. Everyday drugs for pain, allergies, or colds can affect heart rhythm, trigger episodes, or interact with prescribed treatments. For example, research shows that nonsteroidal anti-inflammatory drugs (NSAIDs) may raise the risk of AFib events, especially in older adults or those with heart disease[2]. That’s why it’s important to always check with your doctor and review medication labels, especially when adding or changing anything in your regimen.
Why Avoiding Certain Medications Is Important
Choosing heart-safe medications protects you both immediately and over the long term. By avoiding medicines that can trigger AFib—such as some decongestants, stimulants, or anti-inflammatory drugs—you reduce the likelihood of heart rhythm problems and hospitalization. This also helps your prescribed AFib treatments work more effectively. Discussing all your medication options with your doctor can help you find the safest approach, whether that means the best anticoagulant for AFib or possible non-drug management strategies if appropriate[3].
Common Medications and Supplements to Watch Out For
Several prescription and over-the-counter products can increase the risk of AFib episodes or interact with your treatment:
– NSAIDs (like ibuprofen, naproxen): These can raise blood pressure and worsen heart failure, contributing to AFib[4].
– Decongestants in cold or flu remedies: Products containing pseudoephedrine or phenylephrine may trigger AFib episodes. Always confirm with your doctor before using these[5].
– Stimulant medications (for ADHD or weight loss): These can increase heart rate and blood pressure, raising the risk of arrhythmias for those with AFib[6].
– Certain anti-fungal, antibiotic, or antiarrhythmic drugs: These may interact with blood thinners or other AFib medications, sometimes magnifying risks.
– Herbal supplements and some over-the-counter remedies: Some contain stimulants or interact with your prescription treatments. Always double-check with your doctor or pharmacist.
The Risks of Stopping Medications Abruptly
It is important never to stop taking prescribed AFib medication without medical advice. Abruptly discontinuing your treatment can lead to return of irregular heart rhythms, increased risk of stroke, and possible hospitalization. Changing your medication dose or frequency without your doctor’s guidance could also increase risks[7]. If you experience side effects, talk to your cardiologist about safe adjustments to your treatment plan.
Steps for Safer Medication Management
To help manage AFib safely and effectively:
– Keep an up-to-date list of all medications and supplements you take.
– Share this list with all your healthcare providers, including dentists and pharmacists.
– Always ask about medications that could be risky with AFib—especially before starting any new medicine.
– Review whether any current medication might interact with your anticoagulant or antiarrhythmic therapies.
– Never stop medications suddenly; consult with your doctor about any concerns or side effects.
– Ask about the best anticoagulant options if you require a blood thinner[8].
– Learn about non-drug strategies for managing AFib, such as lifestyle changes or ablation, if you’re exploring alternatives to blood thinners[9].
– Carefully check the labels on cold, allergy, and flu remedies, as these can sometimes trigger AFib.
Small, informed changes in how you approach medications can make a big difference in both your heart health and overall quality of life.
Resources
1. American Heart Association: “Atrial Fibrillation (AF or AFib)”
2. Circulation: “Nonsteroidal Anti-inflammatory Drugs and Risk of Atrial Fibrillation”
3. Mayo Clinic: “Blood Thinners: Options for Atrial Fibrillation”
4. Cleveland Clinic: “NSAIDs and the Heart”
5. Harvard Health Publishing: “Over-the-counter cold remedies and arrhythmias”
6. National Institutes of Health: “Stimulant Use, Arrhythmias, and Potential Risk in Patients with Cardiovascular Disease”
7. MedlinePlus: “Stopping Medications Suddenly Can Be Dangerous”
8. American College of Cardiology: “Anticoagulant Therapy in Atrial Fibrillation”
9. Heart Rhythm Society: “Lifestyle Management and Atrial Fibrillation”
10. FDA: “Drug Interactions: What You Should Know”
