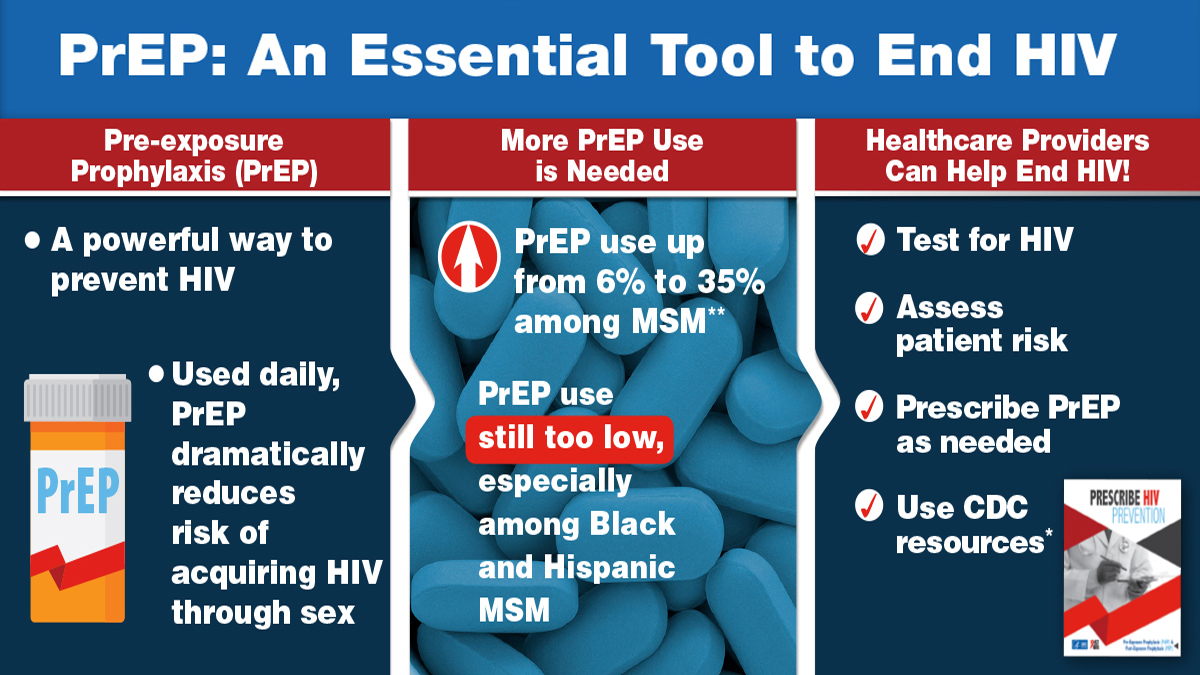
Over the past decade, the global fight against HIV has taken significant strides forward. One of the most groundbreaking developments in HIV prevention is Pre-Exposure Prophylaxis, or PrEP. This medication strategy has been proven to dramatically lower the risk of acquiring HIV in people at higher risk, and its success has reshaped prevention strategies worldwide.
But despite its effectiveness, there is still widespread misunderstanding and misinformation about how PrEP works, who should take it, and what it can and cannot do. This guide aims to break down PrEP in a clear, accessible way—covering what it is, how it works biologically, who can benefit from it, and the role it plays in reducing HIV incidence rates.
1. What is PrEP?
PrEP stands for Pre-Exposure Prophylaxis. It is a preventive treatment for people who do not have HIV but are at risk of being exposed to the virus. The most common form of PrEP is a daily pill that contains two medications: tenofovir disoproxil fumarate (TDF) and emtricitabine (FTC), combined under brand names like Truvada or Descovy.
When taken consistently, PrEP can reduce the risk of acquiring HIV from sexual contact by 99% and from injection drug use by at least 74%. This makes it one of the most powerful tools available for HIV prevention today.
2. How Does HIV Infect the Body?
To understand how PrEP works, it helps to first understand how HIV infects a person.
HIV (Human Immunodeficiency Virus) attacks the body’s immune system, specifically CD4 cells (also called T-helper cells), which help fight infections. Once HIV enters the bloodstream—through unprotected sex, sharing needles, or other exposure—it infects these cells and uses them to replicate itself. Without treatment, HIV can destroy so many CD4 cells that the body can no longer defend itself, leading to AIDS (Acquired Immunodeficiency Syndrome).
3. The Science Behind PrEP
PrEP works by blocking one of the earliest steps in the HIV life cycle.
The drugs in PrEP—TDF and FTC—are nucleoside reverse transcriptase inhibitors (NRTIs). They interfere with reverse transcriptase, an enzyme HIV needs to convert its RNA into DNA inside human cells. Without this conversion, HIV cannot integrate into the host’s genetic material and cannot replicate.
In simple terms:
-
If HIV enters the body, PrEP makes it extremely hard for the virus to take hold and multiply.
-
The drugs work best when present in high enough concentration in the blood and tissues at the time of exposure.
4. How Effective is PrEP?
Numerous studies and real-world data confirm that PrEP is highly effective—but only if taken correctly and consistently.
-
Sexual transmission: Daily PrEP can lower the risk by 99% or more.
-
Injection drug use: Reduces risk by at least 74%.
-
Consistency matters: Missing doses reduces the drug levels in the body, lowering protection.
PrEP’s effectiveness is comparable to, and in some cases even higher than, other major public health interventions, such as birth control pills for preventing pregnancy when taken daily.
5. Who Should Consider Taking PrEP?
PrEP is recommended for people at higher risk of HIV exposure, including:
-
Men who have sex with men (MSM), especially if they:
-
Have condomless sex with partners whose HIV status is unknown.
-
Have multiple sexual partners.
-
Recently had a sexually transmitted infection (STI).
-
-
Heterosexual men and women who:
-
Have an HIV-positive partner.
-
Have multiple partners without consistent condom use.
-
Live in an area with high HIV prevalence.
-
-
People who inject drugs and share needles or other injection equipment.
-
People in serodiscordant relationships (one partner is HIV-positive, the other is not).
6. Types and Forms of PrEP
Currently, PrEP is available in a few main forms:
-
Daily oral pills (Truvada, Descovy): Most common form, taken once daily.
-
On-demand PrEP (2-1-1 dosing): For some men who have sex with men, PrEP can be taken before and after sexual activity instead of daily.
-
Injectable PrEP (Cabotegravir): A long-acting shot given every 2 months, approved in some countries.
7. How to Start PrEP
Starting PrEP involves several steps:
-
HIV Test: To confirm the person is HIV-negative (PrEP is not a treatment for HIV).
-
Kidney Function Test: To ensure the medication is safe for the patient.
-
STI Screening: Recommended as part of overall sexual health.
-
Prescription: Given by a healthcare provider after assessment.
-
Follow-up: HIV testing every 3 months, kidney monitoring, and adherence support.
8. Common Myths About PrEP
Myth 1: “PrEP is only for gay men.”
Fact: PrEP is for anyone at risk of HIV, regardless of sexual orientation.
Myth 2: “PrEP replaces condoms.”
Fact: While PrEP is extremely effective against HIV, it does not protect against other STIs or pregnancy. Condoms are still important for broader protection.
Myth 3: “PrEP causes serious side effects.”
Fact: Most people tolerate PrEP well. Common side effects—like mild nausea or headache—often go away within a few weeks. Serious side effects are rare.
Myth 4: “You can take PrEP only when you think you’ll be exposed.”
Fact: For maximum protection, daily use or proper dosing schedule is required to build and maintain drug levels.
9. Side Effects and Safety
PrEP is generally safe for long-term use.
Possible side effects:
-
Mild nausea, headache, or stomach upset.
-
Small changes in kidney function or bone density (usually reversible after stopping).
Doctors monitor kidney health regularly to ensure ongoing safety.
10. How PrEP Helps Lower HIV Incidence Rates
PrEP has already shown its potential to transform public health.
-
Population-level impact: In cities and countries with high PrEP uptake, new HIV diagnoses have dropped significantly.
-
Breaking transmission chains: Preventing even one infection helps stop onward spread.
-
Empowering individuals: PrEP gives people control over their HIV risk, especially in situations where condom use is not possible or consistent.
For example, in San Francisco, widespread PrEP use contributed to a nearly 50% drop in new HIV infections between 2012 and 2018.
11. Challenges in PrEP Implementation
Despite its effectiveness, challenges remain:
-
Awareness gaps: Many at-risk individuals still do not know about PrEP.
-
Access barriers: Cost, healthcare availability, and stigma can prevent people from starting or continuing PrEP.
-
Stigma and misconceptions: Some people face judgment for using PrEP, wrongly associating it with promiscuity.
-
Adherence issues: Forgetting doses can reduce effectiveness.
12. The Future of PrEP
Research is ongoing to make PrEP more accessible and easier to use:
-
Long-acting implants that last up to a year.
-
Vaginal rings releasing medication over weeks or months.
-
More affordable generic options.
The goal is to integrate PrEP into regular healthcare, making it as routine as other preventive measures like vaccines.
Conclusion
PrEP is one of the most powerful tools available to prevent HIV, offering up to 99% protection against sexual transmission when taken as prescribed. It works by stopping HIV from taking hold in the body, effectively halting infection before it starts.
By expanding awareness, improving access, and addressing stigma, PrEP has the potential to drastically reduce HIV incidence rates worldwide. For individuals at higher risk, PrEP is not just a medication—it is a means of empowerment, giving control over one’s health and future.
