HIV prevention has undergone a transformative shift over the past decade, largely due to the introduction and widespread adoption of pre-exposure prophylaxis (PrEP). Initially supported by randomized clinical trials, PrEP—typically a daily oral medication containing tenofovir disoproxil fumarate (TDF) and emtricitabine (FTC)—has proven to be an exceptionally effective tool in reducing HIV transmission risk. However, as with any public health intervention, its true impact can only be fully understood by examining real-world data.
In the United States, where HIV disproportionately affects certain demographic groups and geographic regions, real-world studies have provided critical insights into PrEP’s effectiveness, uptake, and limitations. This article examines the impact of PrEP on HIV incidence in the US, synthesizing evidence from observational studies, state-level reports, and national surveillance data.
Understanding PrEP and Its Mechanism of Action
PrEP works by maintaining drug levels in the bloodstream and genital or rectal tissues sufficient to block HIV replication if exposure occurs. By inhibiting the HIV reverse transcriptase enzyme, TDF and FTC prevent the virus from integrating into human DNA.
The Centers for Disease Control and Prevention (CDC) recommends PrEP for individuals at high risk of HIV, including:
-
Men who have sex with men (MSM) with multiple partners
-
Heterosexual men and women with HIV-positive partners
-
People who inject drugs (PWID)
-
Individuals with recent sexually transmitted infections (STIs)
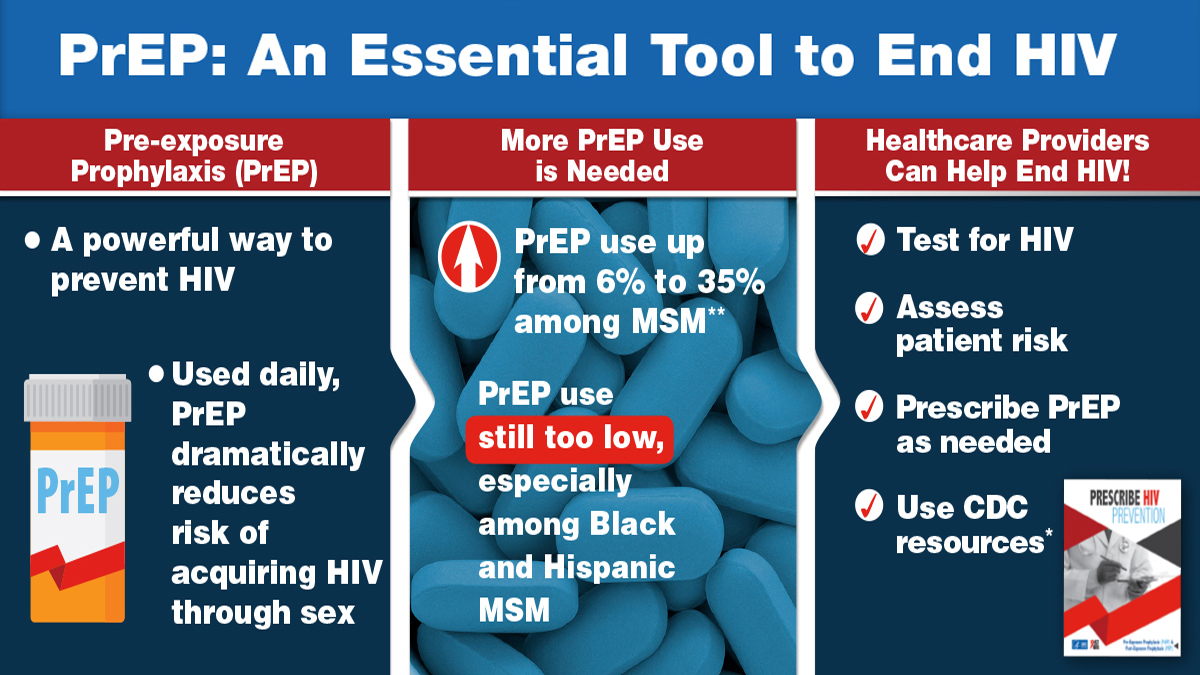
When taken daily, PrEP reduces the risk of acquiring HIV from sexual exposure by about 99% and from injection drug use by at least 74%.
The HIV Landscape in the US Before PrEP
Before PrEP was introduced in 2012, HIV prevention in the US relied heavily on condom promotion, behavioral interventions, and post-exposure prophylaxis (PEP). Despite progress, annual new HIV infections had plateaued at around 38,000–40,000 cases per year.
Certain populations were—and remain—disproportionately affected:
-
MSM account for nearly two-thirds of new infections.
-
Black and Latino communities face higher incidence rates due to structural barriers, stigma, and unequal healthcare access.
-
The Southern US has the highest rates of new HIV diagnoses.
Against this backdrop, PrEP emerged as a biomedical prevention strategy capable of shifting these trends.
Real-World Evidence: Declines in HIV Incidence
1. San Francisco: Early Adoption Success
San Francisco was one of the earliest US cities to promote PrEP aggressively. According to the San Francisco Department of Public Health, HIV incidence dropped by 43% between 2013 and 2016, coinciding with a dramatic rise in PrEP use.
-
By 2017, an estimated 28% of MSM in San Francisco were on PrEP.
-
High adherence levels were reported, correlating strongly with decreased new infections.
2. New York City: Targeted Rollout
In New York City, PrEP uptake among high-risk populations expanded rapidly after 2014. A 2019 city health department report noted a 32% decline in new HIV diagnoses from 2014 to 2018, with the steepest drops among MSM aged 20–29, a group historically at high risk.
3. State-Level Evidence: Washington State
Washington State’s “End AIDS” initiative integrated PrEP distribution into primary care. Studies from 2014–2018 showed a decline in HIV diagnoses among MSM by over 25%, attributed partly to increased PrEP coverage.
The CDC’s National Data on PrEP and HIV Trends
According to CDC surveillance data:
-
National PrEP coverage increased from 3% of eligible individuals in 2015 to 25% in 2021.
-
States with the highest PrEP coverage—California, New York, Massachusetts—saw the largest relative declines in HIV incidence.
-
Conversely, states with low coverage, particularly in the South, experienced smaller declines or plateauing trends.
Factors Driving PrEP’s Real-World Effectiveness
-
High Efficacy with Adherence
Clinical and observational studies consistently show that daily adherence is the key determinant of PrEP’s effectiveness. In real-world settings, those with consistent use experience near-zero HIV seroconversions. -
Integration into Routine Care
When PrEP is offered in primary care, sexual health clinics, and via telehealth, uptake increases substantially. -
Community Outreach and Education
Public health campaigns in cities like San Francisco, New York, and Atlanta have demonstrated that culturally tailored messaging improves both awareness and adoption.
Remaining Challenges in the US
While PrEP’s impact is undeniable, several barriers hinder its full potential:
1. Access and Cost
-
Despite insurance coverage under the Affordable Care Act, co-pays, lab costs, and clinic visits can deter some individuals.
-
Uninsured or underinsured populations—often in rural areas—face the greatest barriers.
2. Geographic Disparities
-
The South, home to over half of new HIV diagnoses, has significantly lower PrEP uptake compared to the Northeast and West Coast.
3. Awareness Gaps
-
Many at-risk individuals remain unaware of PrEP, especially in Black, Latino, and rural communities.
4. Stigma and Misinformation
-
Social stigma associated with HIV, sexual orientation, and PrEP use can discourage uptake.
-
Myths about side effects or “encouraging risky behavior” persist.
Emerging Trends in PrEP Delivery
1. Long-Acting Injectable PrEP
In 2021, the FDA approved cabotegravir (Apretude), an injectable PrEP option administered every two months. Early studies suggest it may improve adherence rates, especially among those who struggle with daily pills.
2. Telehealth Expansion
COVID-19 accelerated the integration of PrEP telehealth services, enabling virtual counseling, at-home HIV/STI testing, and medication delivery.
3. Pharmacy-Based PrEP Access
Some states now allow pharmacists to prescribe and dispense PrEP directly, bypassing traditional clinic barriers.
Evidence-Based Impact: Key Study Summaries
-
Katz et al., 2020 (Washington State)
-
Found a 41% reduction in HIV incidence among MSM correlating with increased PrEP uptake.
-
Concluded that scaling PrEP could significantly reduce incidence nationwide.
-
-
Hughes et al., 2021 (San Francisco)
-
Observed near-zero HIV seroconversions among those adherent to PrEP for over a year.
-
Suggested PrEP as a cornerstone of ending HIV transmission.
-
-
CDC Modeling Study, 2020
-
Estimated that reaching 50% PrEP coverage among eligible individuals could prevent 25,000 new HIV infections over 10 years.
-
Policy Implications
Real-world data make it clear: expanding PrEP access is essential for meeting the Ending the HIV Epidemic (EHE) goal of reducing new infections by 90% by 2030.
Key policy recommendations include:
-
Expanding Medicaid and insurance coverage for PrEP and related services.
-
Funding community-based organizations for targeted outreach.
-
Supporting telehealth and pharmacy-based PrEP models.
Conclusion
PrEP has reshaped the landscape of HIV prevention in the United States. Evidence from cities, states, and national datasets shows that higher PrEP coverage correlates directly with reduced HIV incidence, especially when paired with targeted outreach and strong healthcare integration.
While challenges remain—particularly in access, awareness, and stigma—emerging delivery models such as long-acting injectables and telehealth promise to bridge these gaps. With sustained commitment from policymakers, healthcare providers, and communities, PrEP can play a central role in ending the HIV epidemic in the US.
