1. PrEP Explained: What It Is and How It Works
What Is PrEP?
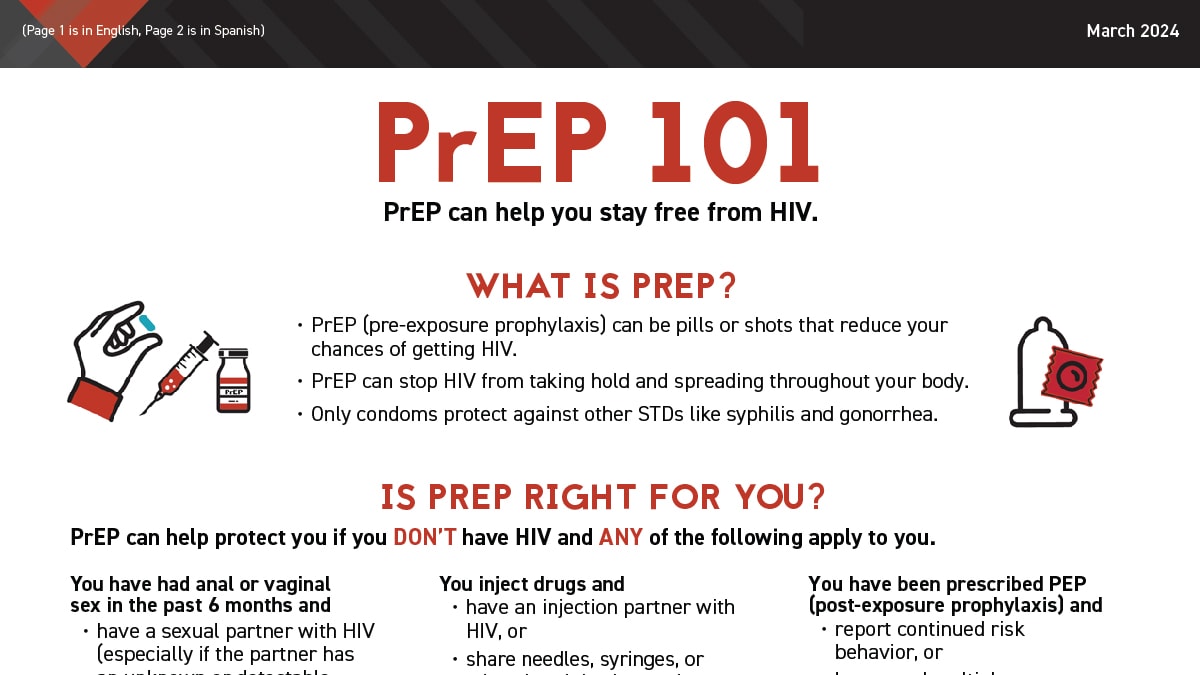
PrEP stands for pre-exposure prophylaxis—a daily or periodic preventive regimen for people who are HIV-negative but at risk of exposure. It works by delivering antiretroviral medication before potential exposure, inhibiting the virus before it can establish infection. Its effectiveness is striking when taken correctly.HIV.govCDCWikipedia
How It Works
PrEP blocks HIV’s ability to replicate after entering the body. The most widely used forms are:
-
Daily oral pills:
-
Long-acting injectable options:
-
Apretude® (cabotegravir)—administered every two months.HIV.govWikipedia
-
Yeztugo® (lenacapavir)—given twice yearly, preceded by two oral doses to achieve protective blood levels.HIV.govThe Washington PostAdelaide Now
-
Just How Effective Is PrEP?
When taken as prescribed:
-
Reduces HIV risk from sex by up to 99%.HIV.govAcogpublichealth.jhu.eduVerywell Health
-
Lowers risk among people who inject drugs by at least 74%.HIV.govpublichealth.jhu.edu
Importantly, effectiveness depends on adherence—the more consistent you are, the better the protection.HIV.govhivinfo.nih.govCDC
2. Who Should Consider PrEP?
Identifying Risk Factors
PrEP is recommended for individuals who:
-
Are HIV-negative and have had anal or vaginal sex in the past six months and either:
-
Inject drugs, especially when sharing gear or with an HIV-positive partnerHIV.govMedlinePlusWikipedia
-
Already received PEP (post-exposure prophylaxis) and have ongoing risk behaviorsHIV.govMedlinePlusdealspot.inauanngon.com
-
Are sexually active, even if not reporting obvious risk factors—many health authorities now recommend discussing PrEP with all sexually active individuals.CDCAcogWikipedia
-
Are pregnant, planning pregnancy, or breastfeeding, and have potential HIV exposure—PrEP may protect both you and your child.HIV.govCDCWikipedia
3. Accessing PrEP: Options, Safety, and Coverage
Medicine Options Summary
| Option | Format | Frequency |
|---|---|---|
| Truvada / Descovy | Oral pill | Daily |
| Apretude | Injection | Every 2 months |
| Yeztugo (lenacapavir) | Injection | Twice yearly |
Safety and Side Effects
-
Generally well tolerated; common mild side effects include nausea, headache, fatigue, and start-up symptoms that resolve quickly.CDCVerywell Health
-
Kidney function may be affected in rare cases with Truvada, especially in older individuals or those with predisposing conditions—monitoring is routine.WikipediaVerywell Health
-
No known harmful interactions between PrEP and hormonal birth control or hormone therapy.CDC
Insurance, Cost, and Assistance
-
Most private insurance and Medicaid are required to cover PrEP services without cost-sharing.The Washington PostCDC
-
Costs vary: generic Truvada can be as low as $30/month, while Yeztugo may cost $14,109 per injection (~$28,218 annually).The Washington Post
-
Assistance programs may soften the financial burden, especially for newer injectables.Adelaide Now
4. Overcoming Barriers to PrEP Use
Common Challenges
Awareness and understanding remain low among both potential patients and healthcare providers.PMCThem
Other obstacles include:
-
HIV stigma, including stereotypes, judgment, or misplaced shame.PMC
-
Healthcare distrust and institutional bias.PMC
-
Limited access to providers who prescribe PrEP or community-based services.PMC
-
Cost concerns—even though many plans cover PrEP, awareness is low.PMCThe Washington Post
-
Difficulty with adherence—especially with daily pills; long-acting options help mitigate this.The Washington PostPMC
Potential Solutions
-
Education campaigns, provider training, and inclusive communication help reduce stigma and increase PrEP awareness.PMCThem
-
Telehealth and pharmacy-based models expand access for underserved populations.PMC
-
Advocacy for equitable coverage ensures newer options like injectables are accessible.The Washington PostAdelaide Now
5. Step-by-Step: How to Start and Sustain PrEP
Step 1: Evaluate Your Risk & Talk to a Provider
Anyone sexually active or sharing needles can ask for PrEP, regardless of perceived risk.CDCWikipedia
Step 2: Complete Baseline Testing & Choose a Regimen
Initial assessments typically include:
-
HIV test (must be negative)
-
Kidney and liver function
-
STI screening
Decide between:
-
Daily oral pill – for convenience and flexibility
-
Injectable (Apretude or Yeztugo) – for minimal dosing burden
Step 3: Stay Engaged & Adherent
-
For pills: take every day, maintain routine check-ins with your provider.
-
For injectables: keep your follow-up appointments (every 2 or 6 months), even if delayed slightly may still be covered.The Washington Post
Step 4: Combine Strategies in a Comprehensive Plan
PrEP is a powerful tool—but should be paired with:
-
Regular condom use (to prevent other STIs and pregnancy)
-
Ongoing STI screening
-
Healthy lifestyle practices
Step 5: Reassess As Needed
Life circumstances, risk levels, and preferences may change. Reevaluate your approach and consult your provider regularly.
6. Looking Ahead: Innovation & Expansion of PrEP
Injectable Breakthroughs
-
Apretude (cabotegravir) has been available since 2021 as a bi-monthly injectable.WikipediaHIV.gov
-
Yeztugo (lenacapavir), approved in 2025, offers biannual dosing and has the potential to transform adherence, particularly for marginalized populations.The Washington PostAdelaide Now
Equity & Global Access
Efforts are underway to expand global access to injectables via funding from international organizations like PEPFAR and the Global Fund, facilitating low-cost availability in lower-income regions.Wikipedia
Future Horizons: Implants, Rings, and Vaccines
-
PrEP research is expanding into new delivery methods—such as implants or vaginal rings.Wikipedia
-
Ultimately, a vaccine may be the most definitive prevention—but until then, PrEP remains our most powerful, accessible tool.The Washington PostThem
Conclusion
PrEP has revolutionized HIV prevention. When used correctly, it delivers nearly 100% protection against HIV infection. Whether through daily pills or cutting-edge injectables like Yeztugo, the options available today are broader and more effective than ever.
Barriers—such as stigma, limited access, and cost—persist. Overcoming them requires education, equitable policy, and stronger healthcare outreach. But for individuals seeking protection and empowerment, PrEP provides a clear path forward.
Talk with a healthcare provider, evaluate your options, and take charge of your sexual health. With understanding and care, you can stay protected—and lead with confidence.
