A Comprehensive Guide to Congenital Adrenal Hyperplasia (CAH) in Women: From Diagnosis to Empowerment
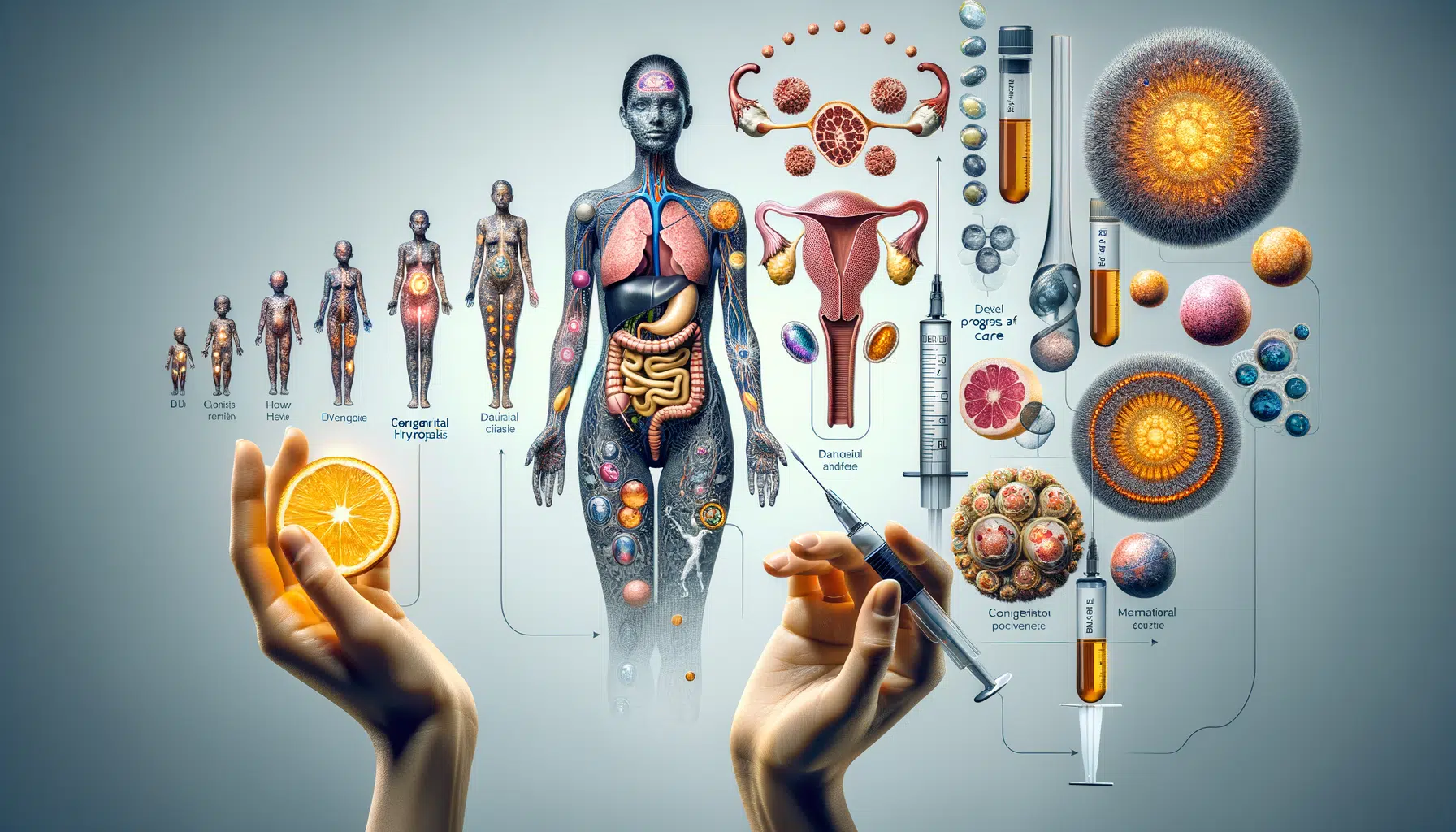
Congenital Adrenal Hyperplasia (CAH) is a complex, inherited endocrine disorder that affects the adrenal glands’ ability to produce crucial hormones. In women, this condition presents a unique and often challenging set of health issues, impacting everything from physical development and hormonal balance to reproductive health and psychological well-being. Understanding the different variants of CAH, recognizing its subtle and overt symptoms, and navigating the path to effective treatment is paramount for those affected. This in-depth guide aims to provide a comprehensive overview of CAH’s impact on women’s health, offering clarity on its classic and nonclassic forms, the risks of untreated symptoms, and the holistic strategies for management.
Classic CAH: Understanding its Bold, Early Beginnings
Classic CAH, the most severe form of the condition, is typically diagnosed at birth or shortly after due to its pronounced symptoms. This variant is a powerful example of how a genetic mutation can fundamentally reshape an individual’s development from the very start. The core issue lies in a deficiency of the enzyme 21-hydroxylase, which is vital for producing cortisol and aldosterone. Without this enzyme, the adrenal glands overproduce androgens, a group of male hormones, leading to a cascade of developmental and physiological changes.
In infancy, a female with classic CAH may present with ambiguous genitalia, a condition where the external sex organs do not clearly appear to be male or female. This is often the first and most immediate indicator of the condition, necessitating prompt medical attention. Throughout childhood, the excessive androgen levels trigger accelerated growth, often making these girls taller than their peers. However, this rapid growth paradoxically leads to premature fusion of the growth plates in their bones, resulting in a shorter final adult height than would otherwise be expected.
Beyond childhood, the effects of untreated classic CAH become even more pronounced. The continued presence of high androgen levels drives significant physiological transformations that extend far beyond cosmetic concerns. These can include voice deepening, the development of male-pattern hair growth (hirsutism) on the face, chest, and back, and persistent, often severe, acne. These physical changes can be distressing and may require careful management. Moreover, the hormonal imbalance can disrupt the entire menstrual cycle, leading to irregular periods (oligomenorrhea) or a complete absence of menstruation (amenorrhea), which in turn has profound implications for a woman’s reproductive potential.
The early onset and pronounced nature of classic CAH demand immediate and consistent medical intervention. The standard treatment involves a regimen of hormone replacement therapy, typically with glucocorticoids (to replace cortisol) and sometimes mineralocorticoids (to replace aldosterone), to balance the body’s hormone levels and mitigate the effects of androgen excess.
Spotting Nonclassic CAH: A Subtle, Yet Significant Challenge
Unlike its classic counterpart, nonclassic CAH (NCCAH) presents a more subtle and nuanced diagnostic puzzle. Symptoms often emerge later in life, typically during adolescence or early adulthood, when hormonal fluctuations are already a natural part of development. This late onset means the condition is often misdiagnosed or overlooked, attributed to more common hormonal issues like Polycystic Ovary Syndrome (PCOS).
The gradual hormonal shifts in NCCAH can manifest in a variety of ways. A young woman might experience precocious puberty, with the early appearance of pubic and armpit hair. As she enters adulthood, she might notice other signs of androgen excess, such as severe, treatment-resistant acne that extends beyond the typical teenage years. Hormonal imbalances can also lead to subtle voice alterations, causing a slight deepening. However, one of the most common and distressing symptoms of NCCAH is menstrual irregularity. Periods may be infrequent, unpredictable, or absent altogether, which often leads to an investigation for other reproductive disorders.
For many women with NCCAH, fertility becomes a significant concern. The same hormonal imbalances that disrupt the menstrual cycle can also interfere with ovulation, making it difficult to conceive. This is a primary reason why many women with the condition are not diagnosed until they seek medical help for infertility. The nuanced nature of these symptoms emphasizes the need for sophisticated diagnostic approaches, often involving hormone level testing, a genetic screen, and careful exclusion of other conditions. The treatment for NCCAH is also less intense than for the classic form and may not be required for all individuals. For those who do require treatment, low-dose glucocorticoids can often be effective in managing symptoms and restoring hormonal balance.
Understanding the Risks of Untreated CAH
While the symptoms of CAH can be physically and emotionally challenging, the true gravity of the condition lies in the risks associated with a lack of treatment. In its classic forms, untreated CAH can precipitate a life-threatening medical emergency known as an adrenal crisis. This crisis occurs when the body, under stress, cannot produce enough cortisol to manage the physiological response. Symptoms are sudden and severe, including persistent vomiting, dehydration, dangerously low blood pressure, and critically low blood sugar levels. Without immediate medical intervention, an adrenal crisis can be fatal.
Infants with the salt-wasting variant of classic CAH face a particularly high risk. The deficiency in aldosterone production means their bodies cannot properly regulate sodium and potassium, leading to severe electrolyte imbalances. This can cause life-threatening dehydration, lethargy, poor feeding, and a failure to thrive. The critical importance of early screening and diagnosis is to prevent these catastrophic outcomes. Newborn screening programs in many countries now include tests for CAH, ensuring that infants can receive a prompt diagnosis and begin life-saving treatment with glucocorticoid and mineralocorticoid replacement therapy.
Even in nonclassic CAH, the lack of management carries risks. The long-term effects of chronic androgen excess can contribute to conditions like insulin resistance, metabolic syndrome, and a higher risk for certain cardiovascular issues. Beyond the physiological, the emotional and psychological toll of living with unmanaged symptoms like hirsutism, acne, and fertility issues can be immense, highlighting the importance of not just physical but also holistic care.
Navigating Reproductive and Hormonal Health
CAH’s most profound impact on women lies in its influence on sexual development and reproductive health. In classic CAH, the exposure to high levels of androgens in utero can lead to the development of ambiguous genitalia, which requires sensitive and expert medical care to ensure the correct gender assignment and to manage any necessary reconstructive surgeries.
In both classic and nonclassic forms, the excess of androgens can disrupt the hypothalamic-pituitary-ovarian axis, the complex hormonal feedback loop that regulates the menstrual cycle. This can lead to irregular periods, anovulation (the absence of ovulation), and an increased risk of miscarriage. For women who desire to have children, managing CAH effectively is a crucial step toward achieving a successful pregnancy. This often involves working with an endocrinologist to optimize hormone levels and may require assisted reproductive technologies.
The hormonal imbalances of CAH can also generate a host of dermatological challenges, including acne and excessive hair growth (hirsutism). These are not merely cosmetic issues; they can deeply affect a woman’s self-esteem and body image. Living with these unexpected physical changes can create a significant disconnect between a woman’s sense of self and her physical appearance, leading to feelings of frustration, anxiety, and social withdrawal. These psychological dimensions of CAH are a core part of the patient experience and require as much attention as the physiological symptoms.
Recognizing the Hidden Indicators of CAH
While classic symptoms are often the focus of medical discussion, CAH can manifest in more subtle ways that are frequently overlooked. A comprehensive understanding of the condition requires an awareness of these hidden indicators.
For some women, the androgen excess might lead to male-pattern baldness or thinning hair on the scalp. This can be a particularly distressing symptom, as it is often unexpected and challenging to treat. Fertility complications, as mentioned earlier, are also a major hidden indicator of NCCAH. Many women are not diagnosed until they begin to seek answers for why they cannot conceive. It is crucial for reproductive endocrinologists to consider CAH as a potential cause for infertility, especially when other conditions have been ruled out.
Beyond the visible, the psychological dimensions of CAH cannot be overstated. The frustration stemming from an unclear diagnosis, the anxiety associated with managing chronic hormonal issues, and the emotional toll of dealing with physical changes that may not align with one’s identity can be immense. Women with CAH may struggle with depression, anxiety, and a feeling of isolation. Comprehensive healthcare for CAH must therefore extend beyond endocrinology to include psychological support and counseling. An interdisciplinary team of specialists, including endocrinologists, gynecologists, and mental health professionals, can provide the holistic care needed to manage this multifaceted condition.
Summary: Unmasking CAH’s Impact and Paving the Way Forward
Congenital Adrenal Hyperplasia is a complex endocrine disorder that profoundly impacts a woman’s health journey. From the pronounced physical manifestations of classic CAH in infancy to the subtle, late-onset symptoms of nonclassic CAH, the condition demands a sophisticated and empathetic approach to healthcare. Recognizing the full spectrum of its effects—from accelerated growth and physiological changes to the profound implications for reproductive and psychological well-being—is the first step toward effective management.
By combining timely medical intervention with a supportive, holistic care model, women with CAH can navigate their unique health challenges with knowledge and resilience. Ongoing education, patient advocacy, and a commitment to interdisciplinary care are essential for empowering those affected to live full, healthy, and confident lives.