Unlike chemotherapy or radiation, which can damage healthy tissues, cell therapy and immunotherapy for cancer diseases offer targeted solutions that aim to eliminate malignant cells while minimizing side effects. This innovation is widely regarded as one of the most important new options for cancer treatment available today.
In this article, we’ll explore how immuno cell therapy works, its role in modern oncology, treatment types, potential benefits, risks, and the success rate of immunotherapy in 2025.
1. What is Immuno Cell Therapy?
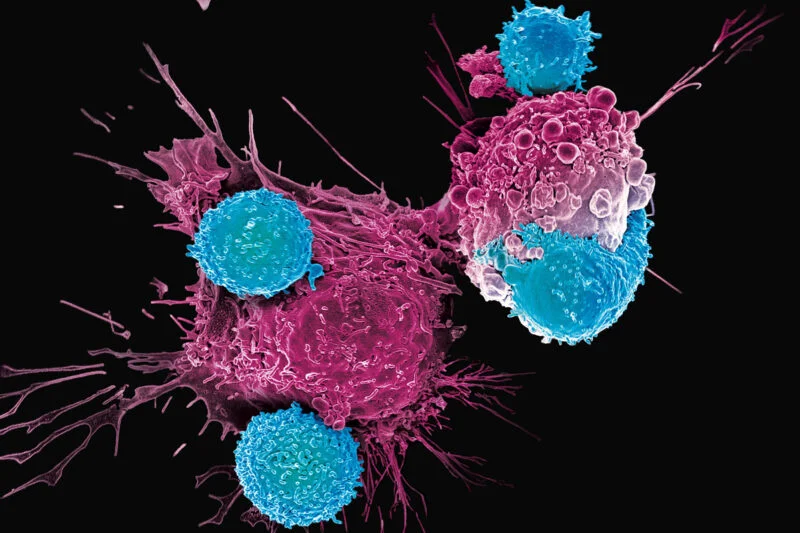
Immuno cell therapy is a type of cancer treatment that uses living immune cells to identify, attack, and destroy cancer cells. These immune cells are collected from the patient (autologous therapy) or from a donor (allogeneic therapy), engineered or expanded in a laboratory, and then infused back into the patient.
The goal is to enhance the natural cancer-fighting ability of the immune system.
Key Features:
-
Personalized to the patient.
-
Targets specific tumor markers.
-
Can provide long-term immune memory, reducing recurrence.
2. Why Immuno Cell Therapy Matters in 2025
Traditional treatments like chemotherapy, radiation, and surgery remain important, but they often fail to completely eradicate cancer or cause significant side effects.
Cell therapy offers several advantages:
-
Precision: Targets tumor cells specifically.
-
Durability: Immune memory cells can prevent relapse.
-
Flexibility: Can be combined with other treatments.
This makes it one of the most promising new options for cancer treatment for various cancer types.
3. Types of Immuno Cell Therapy
a) CAR-T Cell Therapy
-
Stands for Chimeric Antigen Receptor T-cell therapy.
-
T-cells are engineered to recognize cancer-specific proteins.
-
Highly effective in blood cancers like leukemia and lymphoma.
b) TIL (Tumor-Infiltrating Lymphocyte) Therapy
-
Uses immune cells that naturally migrate into tumors.
-
These are harvested, expanded in large numbers, and reinfused.
-
Shown promise in melanoma and cervical cancer.
c) NK (Natural Killer) Cell Therapy
-
NK cells can attack tumors without prior sensitization.
-
Being tested in both blood cancers and solid tumors.
d) Dendritic Cell Therapy
-
Dendritic cells “teach” the immune system to recognize cancer antigens.
-
Used in cancer vaccines like Sipuleucel-T for prostate cancer.
All these approaches fall under the umbrella of immuno cell therapy and represent innovative immunotherapy for cancer diseases.
4. Mechanism of Action
Cancer cells often evade immune surveillance by:
-
Expressing immune checkpoint proteins.
-
Creating an immunosuppressive tumor environment.
Immuno cell therapy counteracts these strategies by:
-
Enhancing T-cell recognition.
-
Boosting immune cell proliferation.
-
Sustaining long-term immune memory.
5. Clinical Applications in 2025
Hematologic Cancers
-
CAR-T therapies are FDA-approved for B-cell leukemia, lymphoma, and multiple myeloma.
-
Survival rates have significantly improved.
Solid Tumors
-
Cell therapy trials are expanding into breast, lung, and pancreatic cancers.
-
Tumor microenvironment challenges remain, but research is progressing.
Preventive and Adjunctive Care
-
Some therapies are combined with checkpoint inhibitors (like PD-1/PD-L1 blockers).
-
Personalized vaccines using dendritic cell therapy are emerging.
6. Success Rate of Immunotherapy
The success rate of immunotherapy varies depending on cancer type, patient health, and treatment stage.
Current Data (2025):
-
CAR-T Therapy: Up to 80–90% remission rates in some blood cancers.
-
TIL Therapy: Around 30–40% response rates in advanced melanoma.
-
Checkpoint Inhibitors (combined with cell therapy): 20–40% durable responses across solid tumors.
While not every patient responds, those who do often achieve long-lasting remission—something rare with conventional chemotherapy.
7. Risks and Side Effects
Like all medical treatments, immuno cell therapy carries risks:
-
Cytokine Release Syndrome (CRS): High fever, low blood pressure due to immune overactivation.
-
Neurotoxicity: Temporary confusion, seizures.
-
Immune System Fatigue: Risk of infections.
However, supportive care and advanced monitoring in 2025 have reduced complications significantly.
8. Accessibility and Cost
One of the main challenges is affordability. Cell therapy can cost hundreds of thousands of dollars per patient. However, biotech companies and insurance providers are working to make it more accessible.
Some governments also support immunotherapy for cancer diseases as part of public health initiatives.
9. Future of Immuno Cell Therapy
The future of immuno cell therapy is promising:
-
Off-the-shelf cell therapies using donor cells (allogeneic CAR-T).
-
Gene-editing technologies like CRISPR to make immune cells stronger.
-
Combination therapies blending chemotherapy, immunotherapy, and targeted drugs.
-
Artificial intelligence in predicting which patients will respond best.
These innovations are expected to improve the success rate of immunotherapy even further in the next decade.
Conclusion
Immuno cell therapy is reshaping oncology by offering patients new options for cancer treatment beyond traditional methods. Whether through CAR-T therapy, NK cell therapy, or dendritic cell therapy, these advances highlight the potential of cell therapy to change cancer care globally.
Although challenges like cost, side effects, and accessibility remain, the rising success rate of immunotherapy proves that we are moving closer to turning once-deadly cancers into manageable chronic conditions.
For patients, families, and healthcare providers, 2025 marks a turning point where hope is backed by science.
References
-
American Cancer Society – Immunotherapy for Cancer
👉 https://www.cancer.org -
National Cancer Institute – Cell Therapy and Immunotherapy
👉 https://www.cancer.gov -
Mayo Clinic – CAR-T Cell Therapy
👉 https://www.mayoclinic.org -
Nature Reviews Cancer – Advances in Immuno Cell Therapy (2024)
👉 https://www.nature.com/nrc -
FDA – Approved Cellular and Gene Therapies
👉 https://www.fda.gov
