In the ongoing global effort to end the HIV epidemic, Pre-Exposure Prophylaxis (PrEP) has emerged as one of the most effective biomedical prevention tools available today. Since its approval by the U.S. Food and Drug Administration (FDA) in 2012, the use of PrEP has expanded significantly, helping to lower HIV incidence rates in many communities.
This article explores what PrEP is, how it works, the science behind its effectiveness, who should consider it, how to access it, and the broader public health implications of widespread PrEP adoption.
1. What is PrEP?
PrEP is a preventive medication regimen taken by HIV-negative individuals to reduce their chances of contracting HIV. It involves the daily use of antiretroviral drugs that stop the virus from establishing an infection if exposure occurs.
Currently, there are two main FDA-approved oral PrEP medications:
-
Truvada® – a combination of tenofovir disoproxil fumarate (TDF) and emtricitabine (FTC), suitable for all individuals at risk.
-
Descovy® – a combination of tenofovir alafenamide (TAF) and emtricitabine (FTC), approved for cisgender men and transgender women but not recommended for those at risk from receptive vaginal sex.
In addition, a long-acting injectable form, Apretude® (cabotegravir), was approved in 2021, offering an option for people who prefer not to take a daily pill.
2. How Does PrEP Work in the Body?
PrEP works by saturating the bloodstream and certain tissues with antiretroviral drugs before HIV exposure occurs. Here’s the process:
-
Step 1: Blocking Reverse Transcriptase
HIV needs an enzyme called reverse transcriptase to copy its RNA into DNA once it enters a human cell. PrEP drugs block this enzyme, preventing the virus from replicating. -
Step 2: Preventing Viral Integration
Without the ability to copy its genetic material, HIV cannot integrate into the host cell’s DNA. This stops the infection process before it can begin. -
Step 3: Creating a Protective Barrier in High-Risk Tissues
The drugs in PrEP accumulate in tissues that are most vulnerable to HIV entry, such as the genital and rectal mucosa, making it much harder for the virus to establish itself.
When taken consistently, PrEP can reduce the risk of acquiring HIV through sexual contact by about 99%, and by at least 74% for people who inject drugs.
3. The Evidence: How Effective is PrEP?
Several large-scale clinical trials have demonstrated PrEP’s effectiveness:
-
iPrEx Study (2010) – Showed a 44% overall reduction in HIV risk among men who have sex with men (MSM), and up to 92% reduction for participants who adhered to daily dosing.
-
Partners PrEP Study (2011) – In heterosexual couples where one partner was HIV-positive, PrEP reduced infection risk by 75%.
-
Bangkok Tenofovir Study (2013) – Demonstrated a 49% reduction in HIV risk among people who inject drugs, with higher efficacy linked to adherence.
-
HPTN 083 and 084 Trials (2020) – Showed that injectable cabotegravir was even more effective than oral PrEP in some populations.
Key takeaway: PrEP works best when taken consistently as prescribed. Skipping doses can lower drug levels in the body, reducing its protective effect.
4. Who Should Consider PrEP?
According to the U.S. Centers for Disease Control and Prevention (CDC), PrEP is recommended for individuals who are HIV-negative and at substantial risk, including:
-
Sexual exposure risk:
-
Men who have sex with men (MSM) who have had condomless sex or a sexually transmitted infection (STI) in the past six months.
-
Heterosexual men and women with an HIV-positive partner or multiple partners whose HIV status is unknown.
-
Individuals who engage in transactional sex.
-
-
Injection drug use risk:
-
People who share needles or other injection equipment.
-
Those in drug-using networks where HIV is prevalent.
-
-
Other considerations:
-
People who have been prescribed post-exposure prophylaxis (PEP) more than once in the past year.
-
Individuals living in communities with high HIV incidence rates.
-
5. How to Start PrEP
Starting PrEP involves several steps to ensure safety and effectiveness:
-
Initial HIV Test – To confirm HIV-negative status. PrEP should not be started if you are already HIV-positive.
-
Kidney Function and Hepatitis B Screening – Tenofovir can affect kidney function, and PrEP may impact hepatitis B treatment.
-
Prescription from a Healthcare Provider – You’ll receive either oral pills or injectable medication.
-
Follow-Up Visits Every 3 Months – These include HIV testing, STI screening, and prescription refills.
6. Types of PrEP Regimens
-
Daily Oral PrEP – The most common form, ideal for those who can maintain consistent pill-taking habits.
-
On-Demand or “2-1-1” PrEP – An alternative dosing method for cisgender MSM, involving two pills 2–24 hours before sex, one pill 24 hours later, and another 48 hours later. Not approved in all countries and not recommended for vaginal sex or injection drug use.
-
Injectable PrEP – Cabotegravir injections every two months, ideal for those who prefer not to take daily pills.
7. Safety, Side Effects, and Misconceptions
Side effects of PrEP are generally mild and temporary, including nausea, headaches, and slight decreases in kidney function or bone mineral density. Most resolve within the first month.
Common misconceptions:
-
“PrEP is only for gay men.” – False. PrEP is for anyone at risk of HIV, regardless of sexual orientation or gender identity.
-
“PrEP replaces condoms.” – Not entirely. While PrEP is highly effective against HIV, it does not protect against other STIs like gonorrhea or chlamydia.
-
“PrEP is too expensive.” – In the U.S., most insurance plans cover PrEP, and assistance programs are available for those without insurance.
8. Public Health Impact
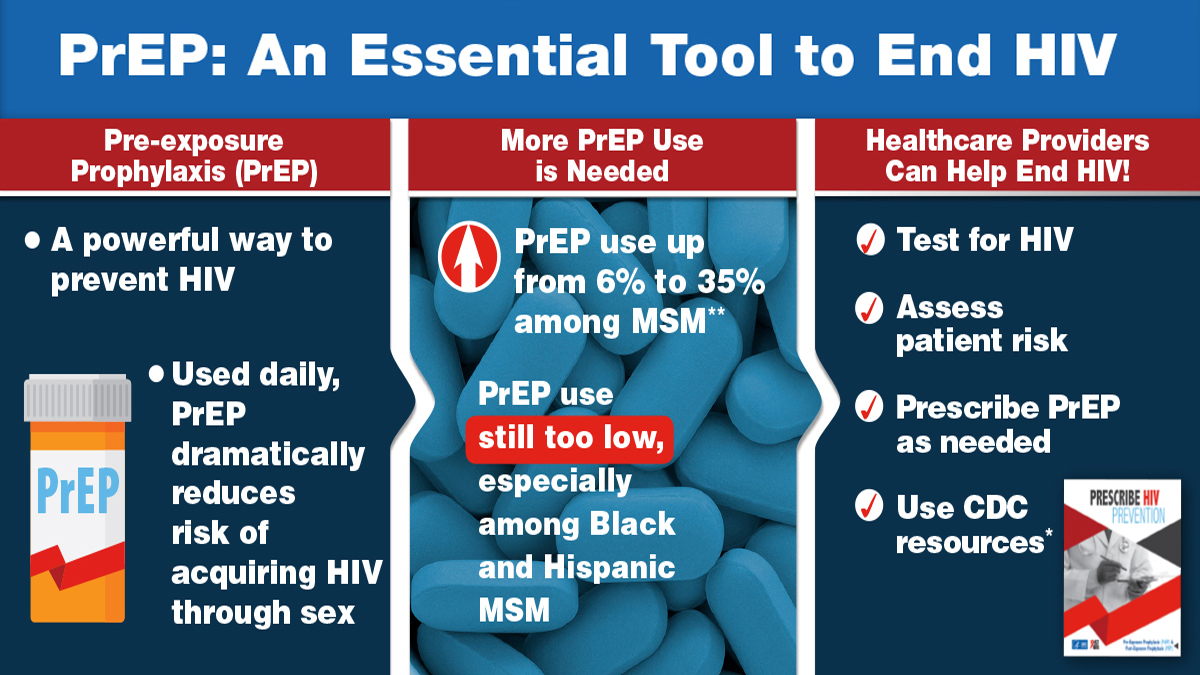
The widespread adoption of PrEP has the potential to drastically reduce new HIV infections, especially when combined with other prevention strategies like condom use, regular testing, and early treatment for people living with HIV.
For example:
-
Cities like San Francisco and Sydney have reported significant drops in HIV incidence after scaling up PrEP access.
-
Mathematical models predict that if just 25% of high-risk individuals in the U.S. used PrEP, new HIV cases could be cut in half within a decade.
9. Barriers to Access
Despite its proven benefits, PrEP uptake remains lower than ideal due to:
-
Stigma surrounding HIV and sexual health.
-
Limited awareness among both the public and healthcare providers.
-
Cost and insurance barriers in certain regions.
-
Geographic gaps in availability, particularly in rural areas.
Addressing these barriers through education, policy changes, and telehealth services can help more people benefit from PrEP.
10. How to Access PrEP Near You
Step 1: Check with your primary care provider or a local sexual health clinic.
Step 2: Search online for “PrEP services near me” – many clinics offer same-day prescriptions.
Step 3: Explore online PrEP providers like Nurx, Mistr, or PlushCare, which offer telehealth consultations, lab testing, and home delivery.
Step 4: If cost is an issue, apply for assistance through Gilead’s Advancing Access® program or local public health initiatives.
11. The Future of PrEP
Research is ongoing to develop more convenient and accessible PrEP options, including:
-
Implants that release medication for up to a year.
-
Microneedle patches for painless self-administration.
-
Broadly neutralizing antibodies (bNAbs) as an alternative to current antiretroviral drugs.
These innovations aim to make HIV prevention even more effective and user-friendly.
Conclusion
PrEP is a game-changing tool in the fight against HIV. By blocking the virus before it can take hold in the body, it offers near-complete protection for those who take it consistently. Its success depends on awareness, accessibility, and adherence — and as more people understand and trust PrEP, the goal of ending the HIV epidemic becomes increasingly achievable.
If you believe you might benefit from PrEP, speak with a healthcare provider or explore online prescription services. Your choice to start PrEP could protect not only your own health but also help reduce HIV transmission rates in your community.
