What is Congenital Adrenal Hyperplasia?
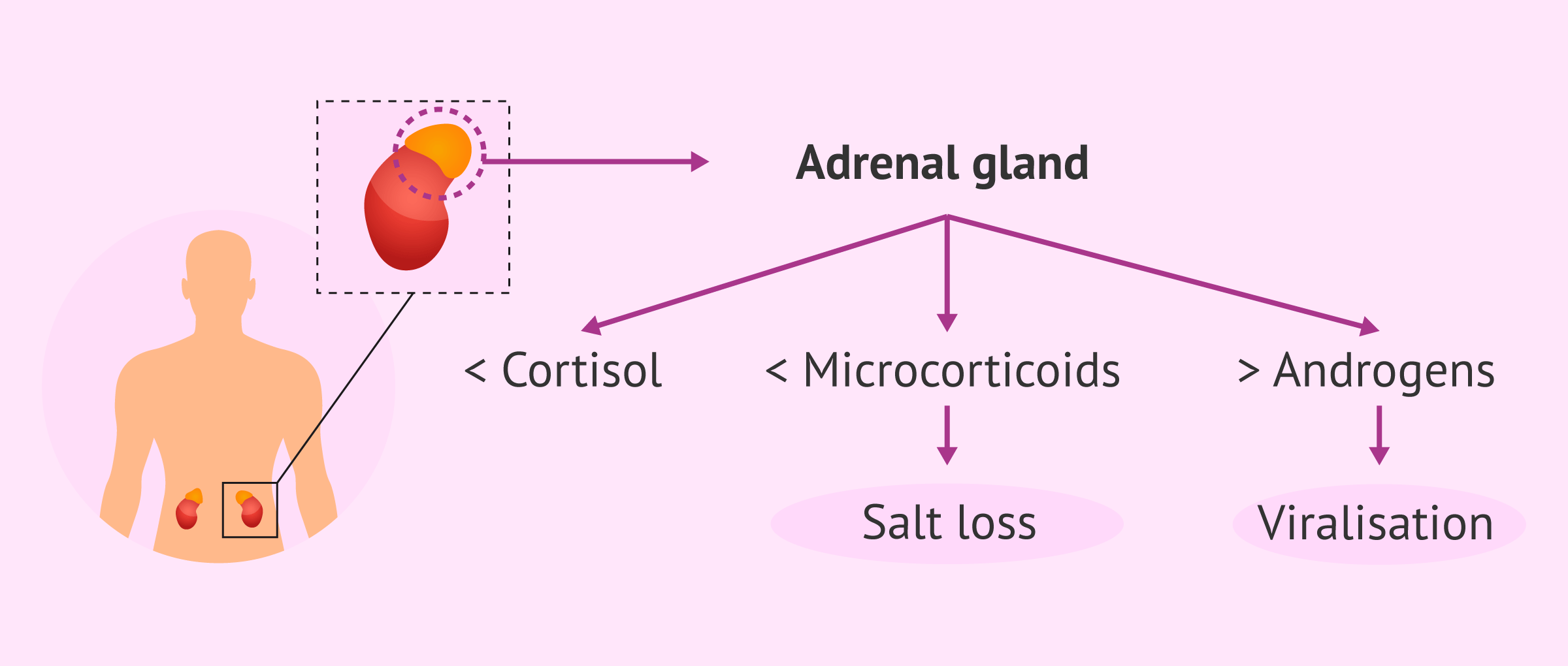
Congenital adrenal hyperplasia is an inherited condition causing imbalance in hormone production due to enzyme deficiencies, most commonly 21-hydroxylase. This enzyme deficit impairs cortisol production and prompts adrenal glands to increase androgen hormone production. Excess androgen results in a spectrum of symptoms, varying greatly based on severity. While classic CAH is usually identified at birth, non-classic CAH can appear subtly and often goes unnoticed until adulthood—a condition known as late-onset congenital adrenal hyperplasia. In females, non-classic CAH symptoms in adult women are frequently mistaken for other hormonal disorders such as polycystic ovary syndrome (PCOS). A significant question arises on PCOS vs non-classic CAH symptoms, since both conditions involve menstrual irregularities, excessive hair growth, acne, and fertility concerns, yet require distinctly different management approaches [1].
Recognizing Often-Overlooked Symptoms
Many women with late-onset CAH remain undiagnosed well into adulthood. Unexpected signs of CAH in women may include irregular or absent menstrual periods, fertility problems, persistent acne unresponsive to common treatments, or excessive facial and body hair growth. Fatigue, mood swings, and low stress tolerance are also easily overlooked symptoms of CAH in females. Considering these nuanced signs can prompt timely clinical evaluation, preventing potential complications from untreated CAH such as osteoporosis, infertility, cardiovascular disease, and increasingly pronounced androgen features [2].
Diagnosis: Identifying Late-Onset CAH
Women experiencing characteristic symptoms may wonder, “how is late-onset congenital adrenal hyperplasia diagnosed?” Accurate diagnosis involves comprehensive clinical evaluation, medical history, physical examination, adrenal hormone blood tests—including measuring serum 17-hydroxyprogesterone levels—and genetic testing to confirm enzymatic defects [3]. Clarifying CAH diagnosis from similar hormonal disorders such as PCOS ensures women receive correctly targeted care strategies.
Navigating Treatments and Fertility Management
Multiple comprehensive congenital adrenal hyperplasia fertility treatment options can substantially improve reproductive outcomes. Standard therapy usually encompasses hormonal therapy, typically glucocorticoids (such as hydrocortisone) to reduce androgen excess and regulate menstrual cycles, fertility medications to enhance ovulation, and—when indicated—assisted reproductive technologies [4]. Continuous advancements in medical research are unveiling exciting new therapies. The latest treatments for CAH include emerging steroid hormone analogs designed specifically to precisely manage CAH-related hormone imbalances while potentially reducing long-term side effects of glucocorticoid therapy for CAH [5].
Addressing Psychological and Emotional Health
It’s essential to acknowledge congenital adrenal hyperplasia and mental health in women. CAH carries potential psychological impacts due to hormone fluctuations, fertility challenges, body image concerns, and societal misunderstandings. It’s natural that women affected by CAH frequently experience stress, anxiety, depression, or decreased self-esteem. Additionally, the emotional component becomes even more relevant when managing CAH during pregnancy, as the condition can complicate conception, gestation, and postpartum well-being [6]. Professional mental health support and peer networks are critical sources of strength. Access to counseling, CAH-focused support groups, and awareness of emotional health needs can significantly reduce anxiety, improve coping strategies, and enhance overall quality of life.
Practical Lifestyle Management and Preparing for Challenges
Effective lifestyle management for congenital adrenal hyperplasia combines medical treatment with careful attention to diet, physical activity, and stress-reduction techniques. Balanced nutrition and weight management can significantly minimize symptom severity. Regular exercise helps strengthen bones and muscles—useful in reducing risks of long-term steroid use such as osteoporosis. Consistent sleep routines and mindfulness practices benefit emotional stability and resilience [7]. Navigating insurance coverage for CAH treatment poses unique challenges, as policies covering specific genetic conditions and newer treatments vary widely in their details. Women and families must advocate proactively, consulting healthcare providers to effectively document medical necessity for treatments while collaborating closely with insurers’ representatives.
Risks of Untreated Non-Classic CAH in Females
Awareness is crucial—ignoring or neglecting proper management can lead to severe risks of untreated non-classic CAH in females. Chronic androgen overproduction can prompt long-term issues including severe fertility impairment, metabolic dysfunction, heightened cardiovascular risks, anxiety, depression, and impaired bone density. It’s critical that individuals receive a timely diagnosis and adhere closely to a tailored treatment approach to mitigate these risks [8]. CAH is a complex health condition, but with proper knowledge, personalized treatments, psychological support, and lifestyle adjustments, women can lead thriving and healthy lives.
