For many, the path begins with confusion rather than clarity: irregular periods, unexplained acne, persistent fatigue, or heartbreaking struggles with fertility. What seems like a series of disconnected symptoms often turns out to be threads of the same story—one that modern medicine is now helping women untangle and reclaim.
Early Signs: When Symptoms Speak in Whispers
CAH rarely announces itself loudly at first. For some women, the earliest sign is seen at birth, when doctors investigate ambiguous genitalia. But in nonclassic cases, the clues remain hidden until adolescence or adulthood.
Common signals include:
-
Menstrual cycles that remain irregular far beyond teenage years.
-
Acne that resists every cream, pill, or lifestyle change.
-
Unexpected hair growth on the chin, chest, or back.
-
Voice changes or thinning hair at the crown.
-
Challenges with conception despite trying for months or years.
Because these signs overlap with more common conditions like Polycystic Ovary Syndrome (PCOS), many women face years of unanswered questions. This delay often leaves them feeling overlooked, misunderstood, or even dismissed.
Diagnosis: Finding the Missing Piece
Finally putting a name to the condition is often life-changing. Diagnosis typically involves:
-
Hormone tests revealing elevated 17-hydroxyprogesterone and androgens.
-
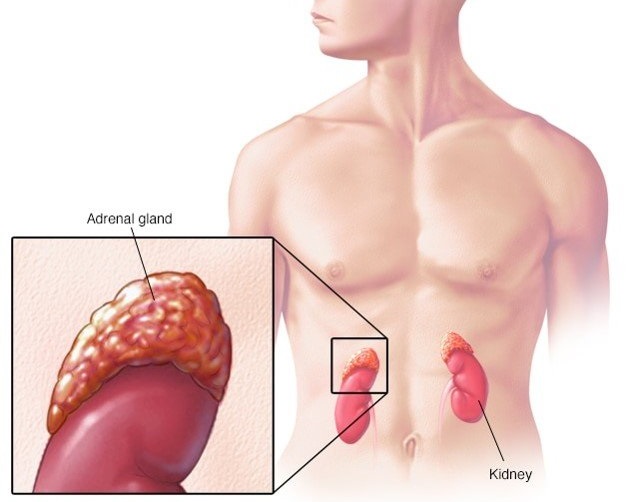
ACTH stimulation tests showing how the adrenal glands respond under stress.
-
Genetic testing confirming mutations in the CYP21A2 gene.
-
Imaging when needed to rule out other conditions.
For many women, diagnosis is a moment of both relief and reckoning—relief in finally understanding their body, yet anxiety about what the future holds.
Treatment: Restoring Balance and Hope
The cornerstone of CAH care is hormone replacement therapy, designed to restore balance and reduce the impact of excess androgens. This may include:
-
Glucocorticoids, to replace cortisol and manage hormone imbalance.
-
Mineralocorticoids, in salt-wasting cases, to regulate essential electrolytes.
-
Stress dosing, with higher medication during illness, surgery, or high-stress events.
Treatment is not just about numbers on a lab report—it’s about reclaiming normalcy: regular cycles, improved skin, reduced hair growth, and renewed chances of motherhood.
Fertility and Family Dreams
For women with CAH, the idea of building a family can feel daunting—but today, it is more possible than ever.
-
Glucocorticoid therapy can restore ovulation and natural fertility in many women.
-
Assisted reproductive technologies (ART), such as IVF, provide additional pathways.
-
Careful monitoring during pregnancy allows many women with CAH to deliver healthy babies.
With the right team of endocrinologists and fertility specialists, dreams of motherhood do not have to fade—they can be realized.
Beyond Hormones: The Emotional Battle
CAH doesn’t just affect the body—it shapes self-esteem, confidence, and mental well-being. Symptoms like unwanted hair growth or irregular cycles can quietly erode a woman’s sense of self.
That’s why emotional care is as important as medical care:
-
Therapy and counseling help women navigate anxiety, self-image, and fertility concerns.
-
Peer support groups provide a space to share stories and strength.
-
Education and advocacy empower women to take charge of their care instead of feeling powerless.
Addressing these inner battles allows women not only to manage CAH but to rise above it.
The Future of CAH Care
Research is paving the way for breakthroughs that may one day transform treatment:
-
Modified-release hydrocortisone better mimics the body’s natural rhythm.
-
Gene therapy is being studied as a potential long-term solution.
-
Personalized medicine is tailoring care to each woman’s unique genetic profile and lifestyle.
The future promises not just survival, but a fuller, freer life for women with CAH.
Living Fully with CAH
Managing CAH successfully means integrating care into daily life—without letting it define who you are. Many women thrive by embracing:
-
Regular check-ups with endocrinologists.
-
Balanced diet and exercise, supporting both hormone health and overall wellness.
-
Stress management practices, from yoga to mindfulness, reducing the body’s cortisol demands.
-
Self-advocacy, asking questions and shaping their own healthcare journey.
CAH may be part of a woman’s story, but it does not have to be the whole story.
Conclusion: From Struggle to Strength
Congenital Adrenal Hyperplasia is more than a medical condition—it is a challenge that women meet with courage, adaptability, and resilience. From delayed diagnoses to modern breakthroughs, from struggles with identity to victories in family planning, the CAH journey reflects strength in its purest form.
With medical progress, emotional support, and empowered voices, women with CAH are proving that they are not defined by their condition. Instead, they are writing new narratives of strength, hope, and possibility.
